Chapter 4 of 6
Treatment Planning
After placing fields and defining field borders, the next step is to calculate the dose and assess the resulting dose distribution.
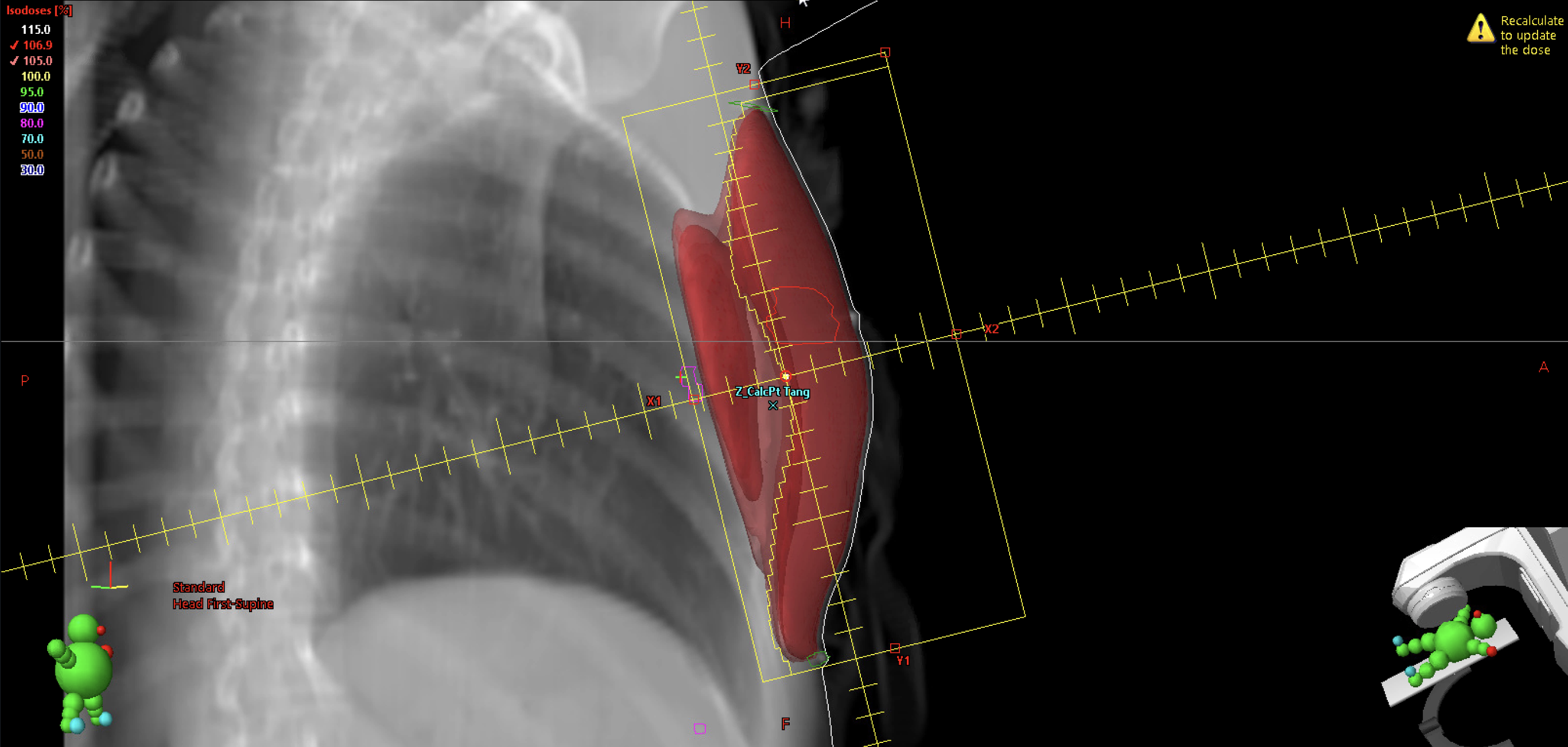
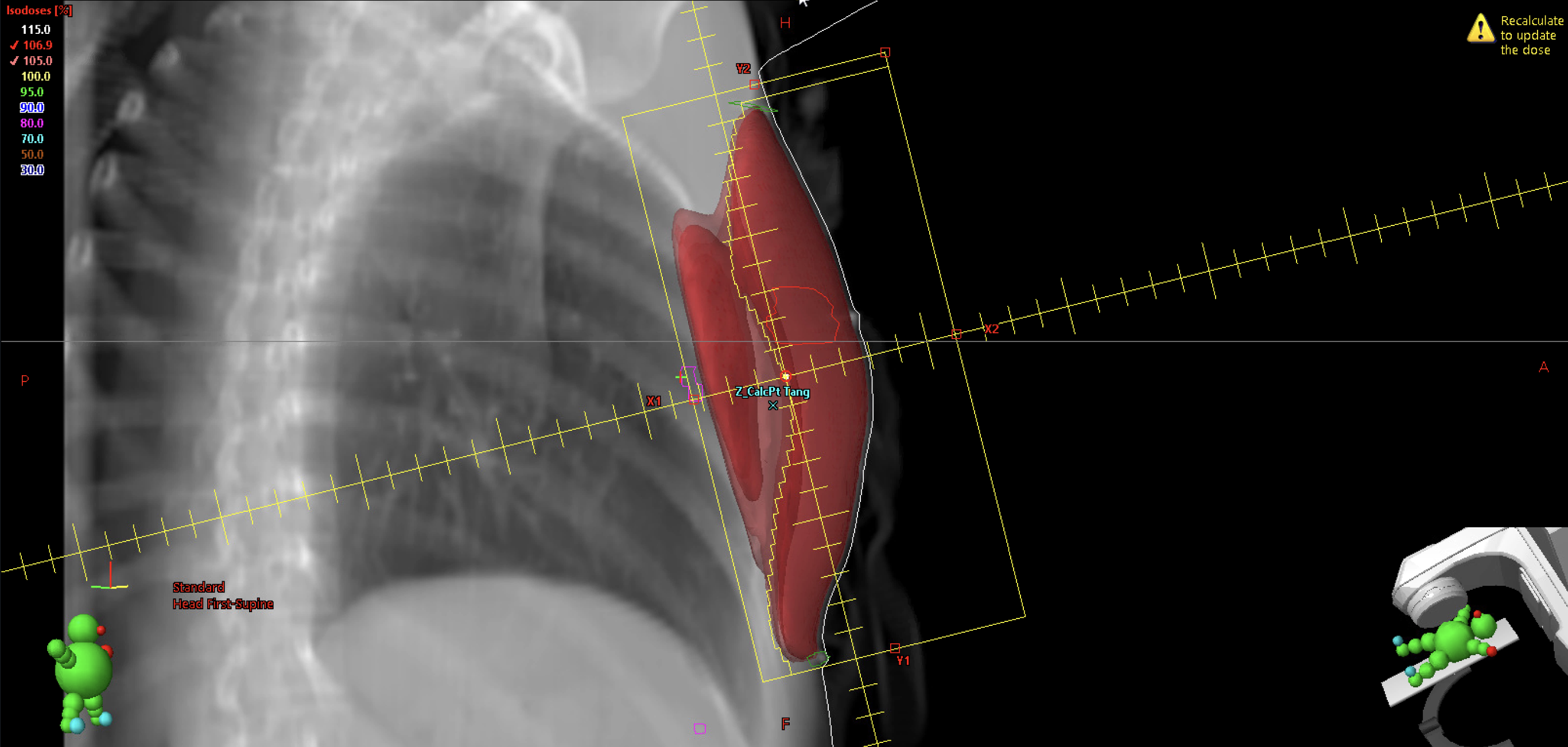
Calculation Point
In some treatment planning systems, a calculation point is not required for planning. However, adding one may be beneficial for other purposes, such as secondary monitor unit (MU) verification by physics staff.
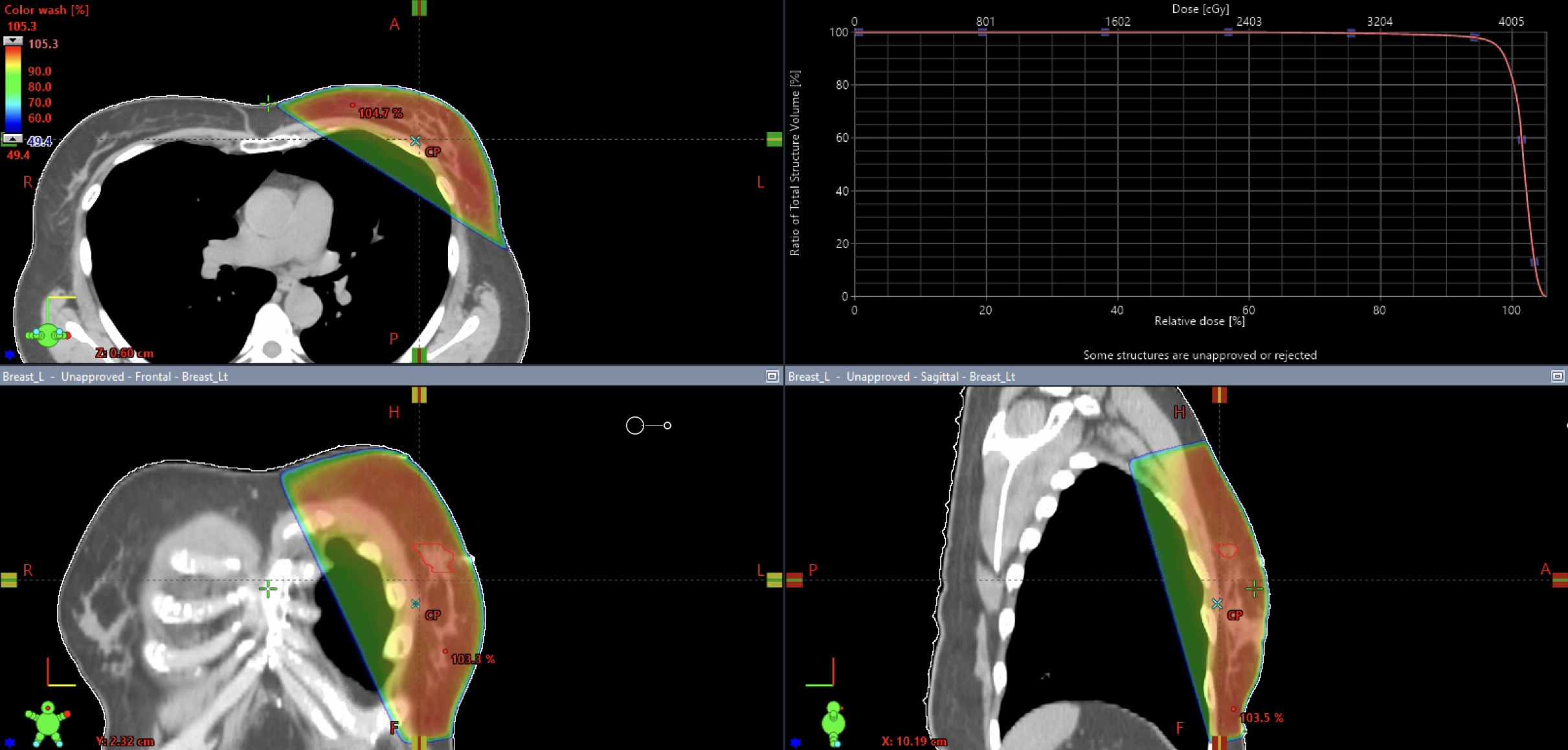
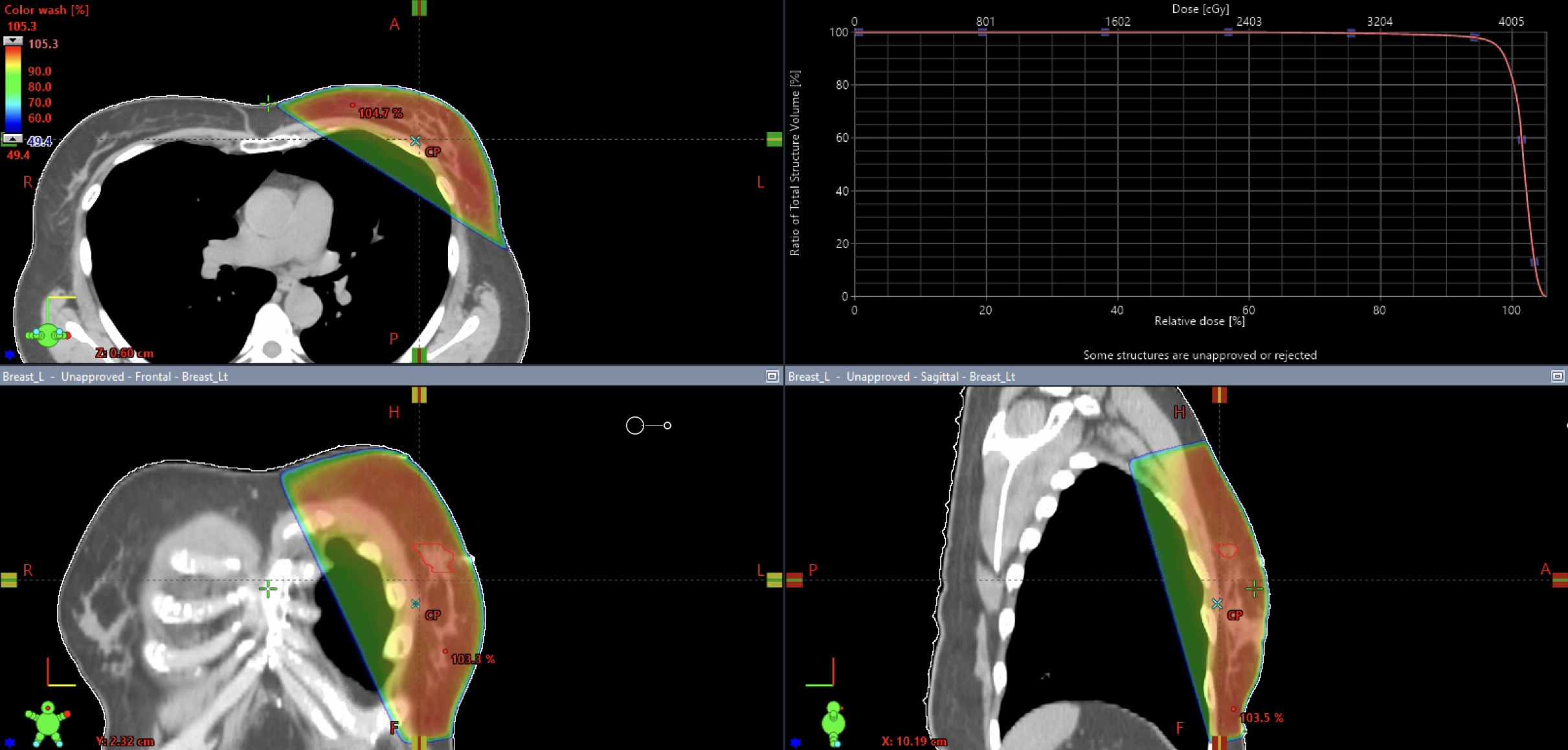
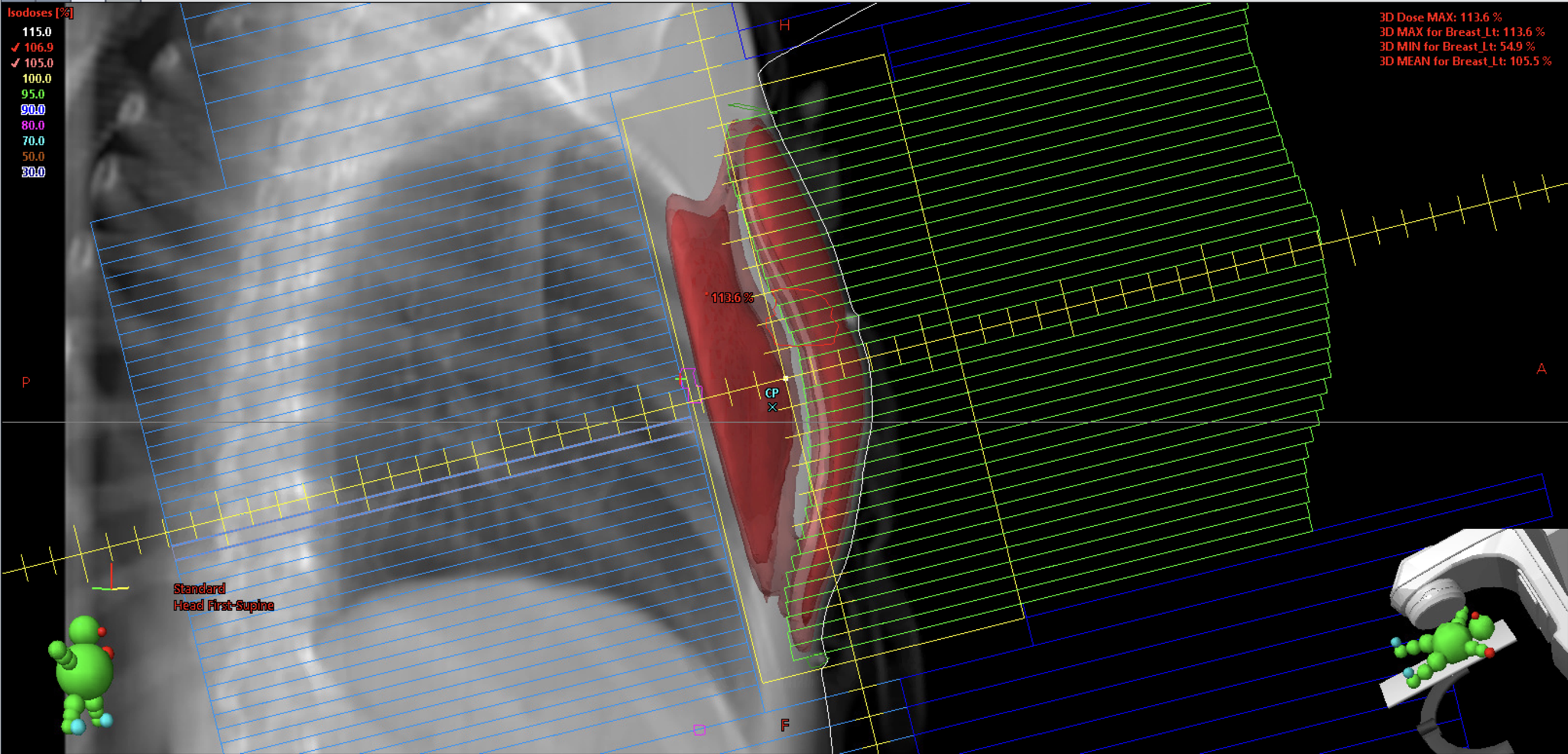
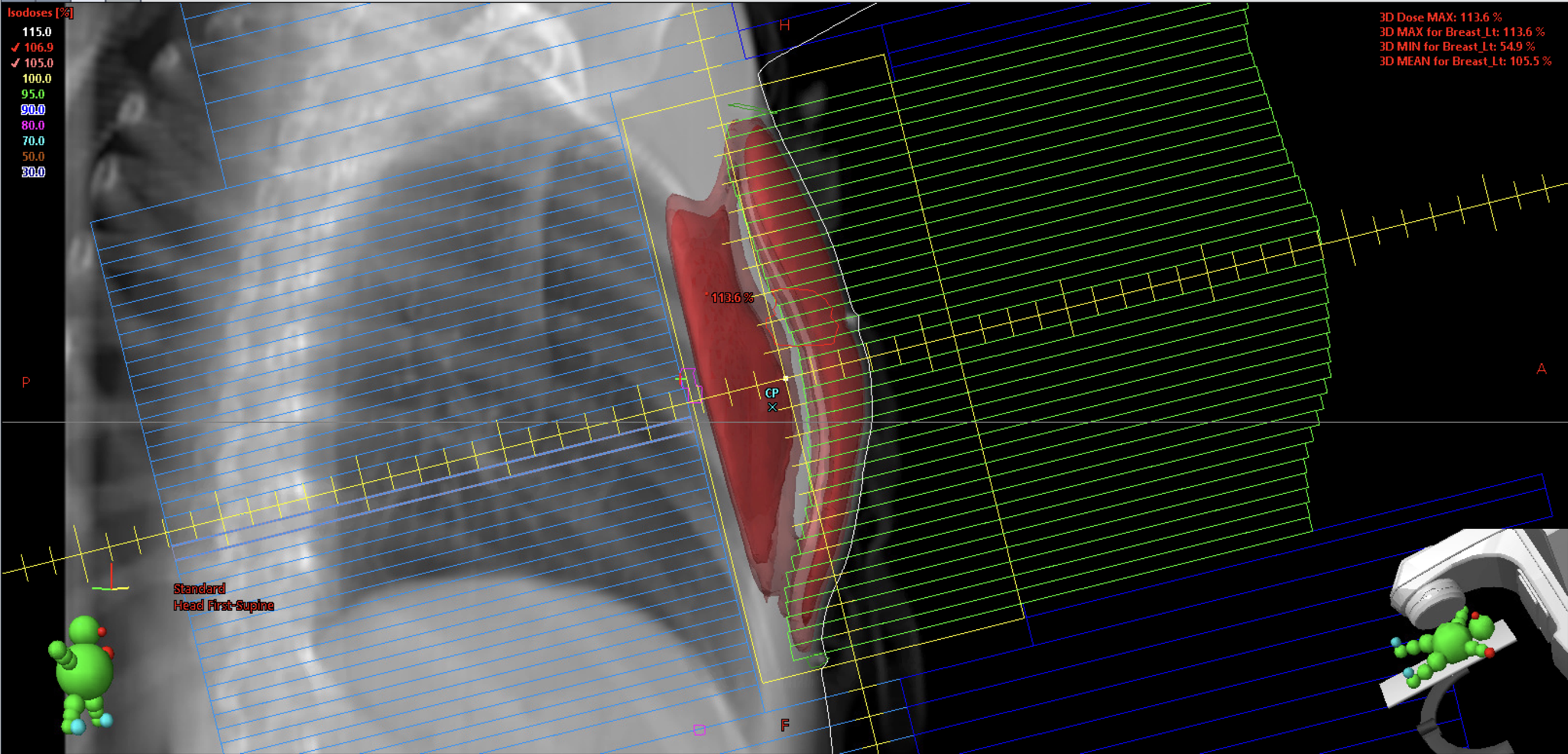
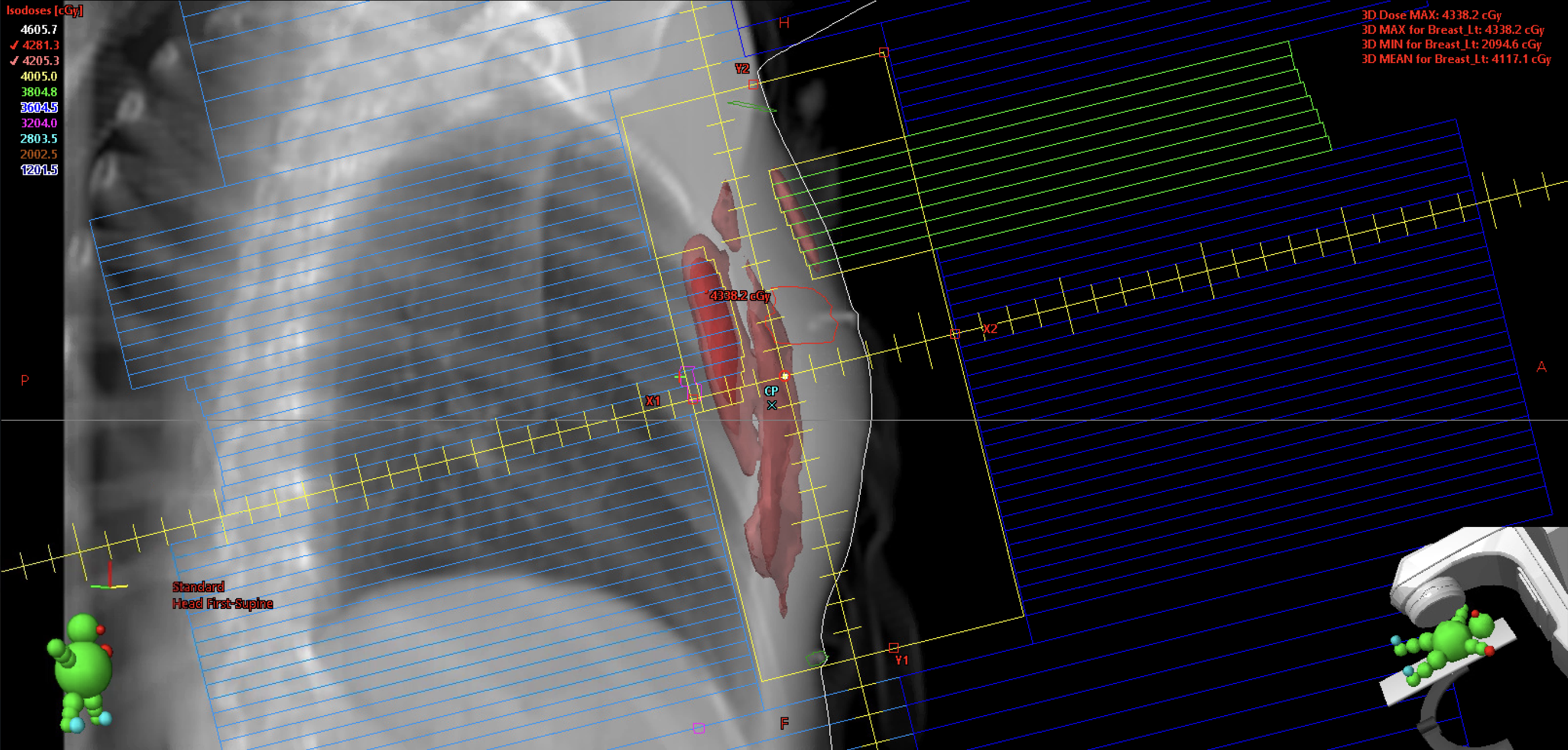
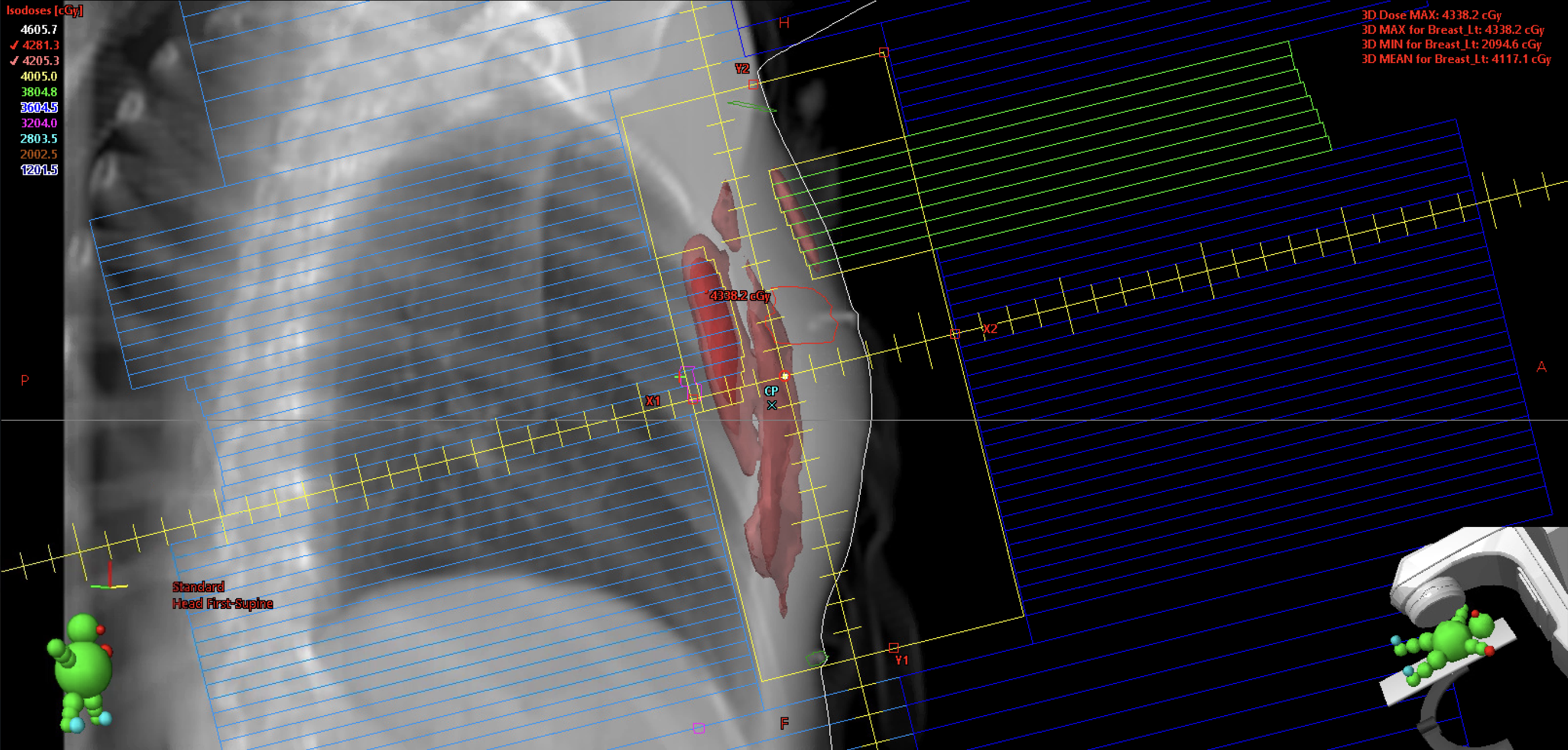
Below is an example of an optimal location for the calculation point.
Field Weighting
Field weighting is used to achieve a uniform dose distribution throughout the treatment area, minimizing hotspots both medially and laterally. If the calculation point or isocenter is positioned at mid-separation, the weighting between the medial and lateral fields is typically 50/50. However, slight adjustments toward one field may be necessary to fine-tune and balance the dose distribution.
To enhance the distribution, adjust the field weighting as needed. If weighting alone is insufficient, as in this example, consider increasing the dose by normalizing the plan and reevaluating the dose distribution.
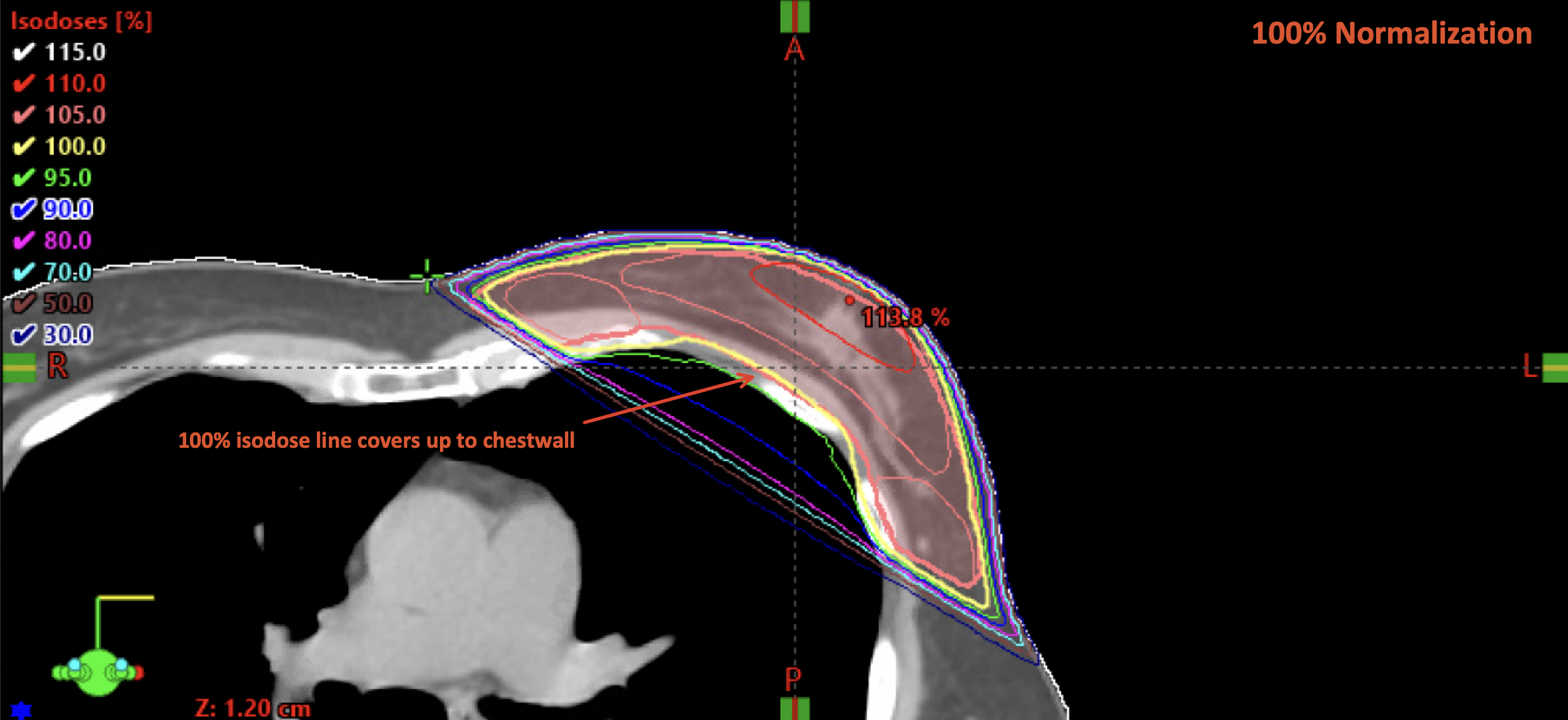
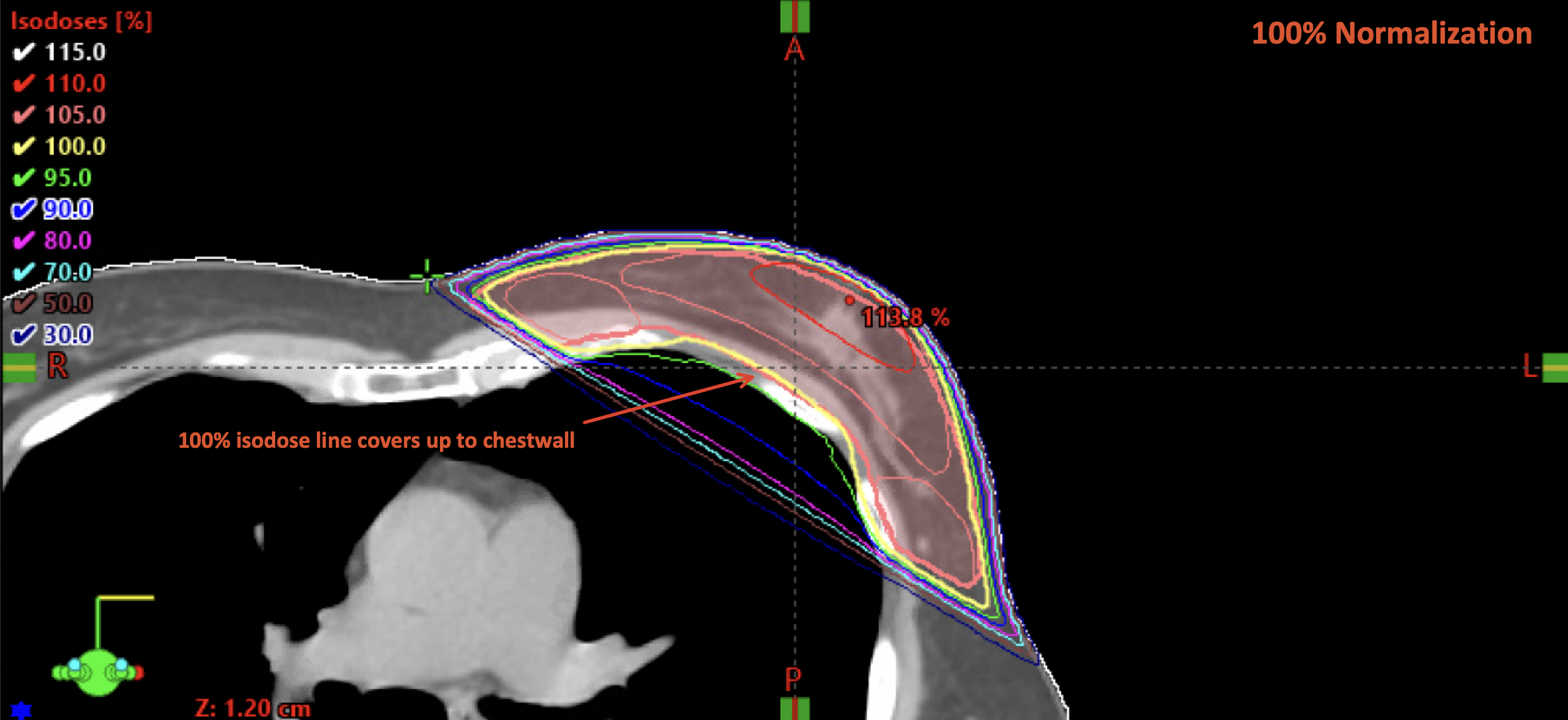
Plan Normalization & Coverage
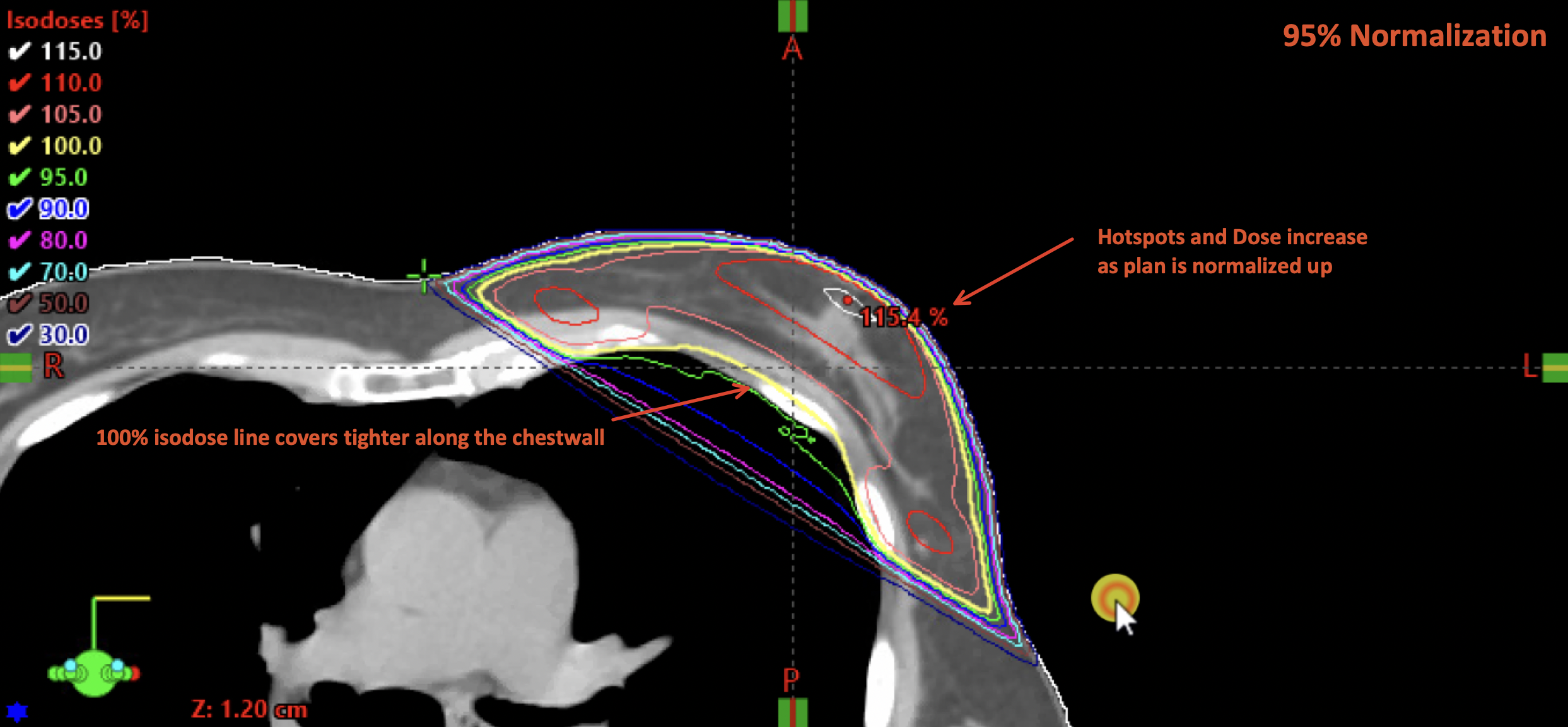
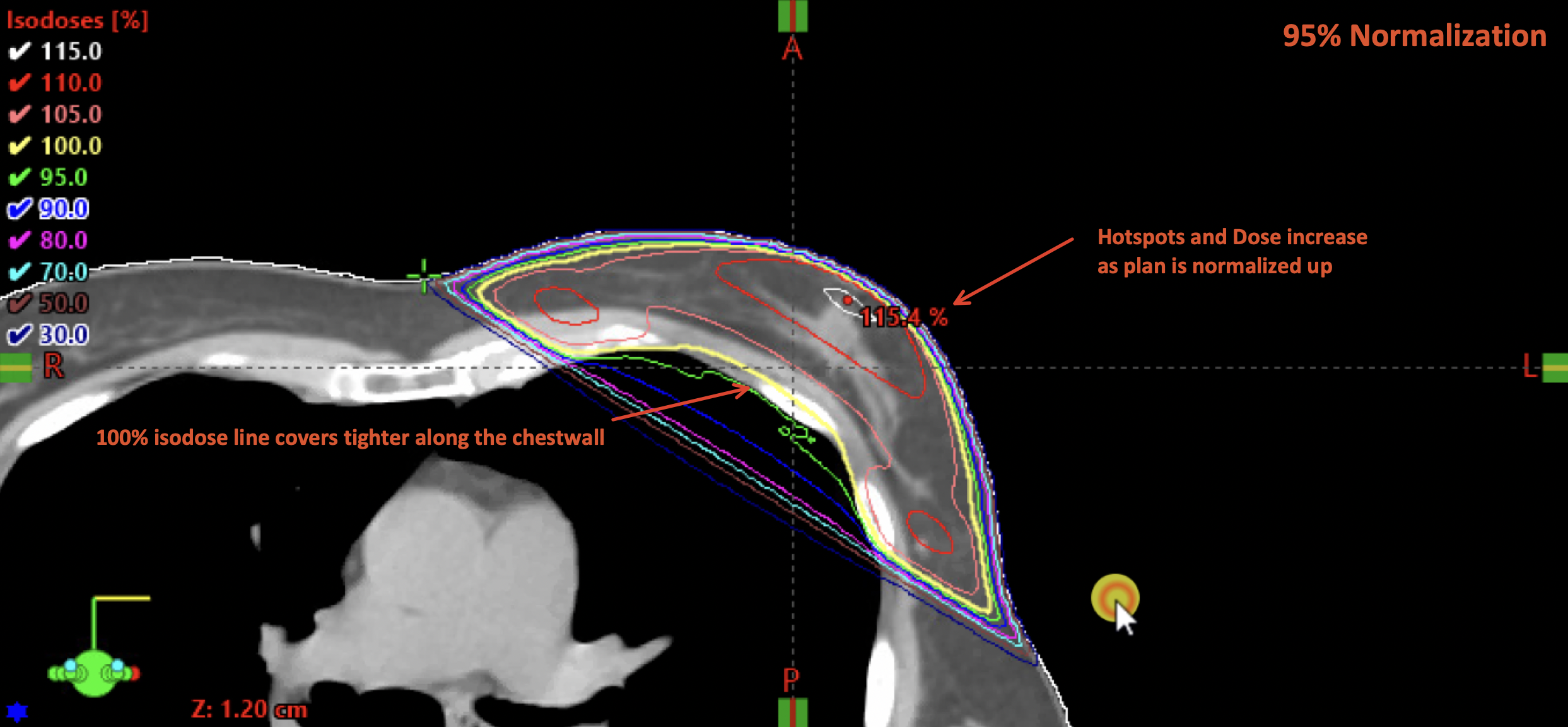
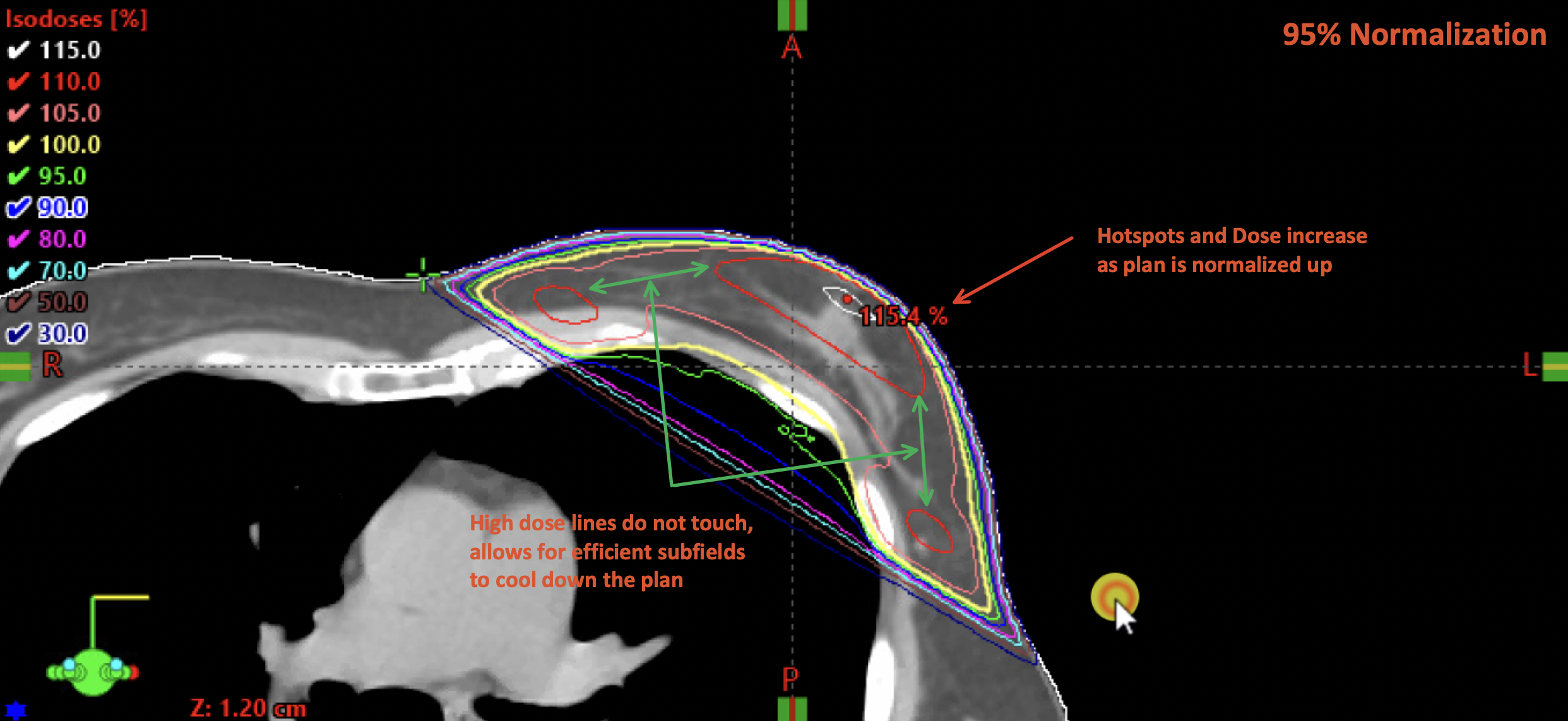
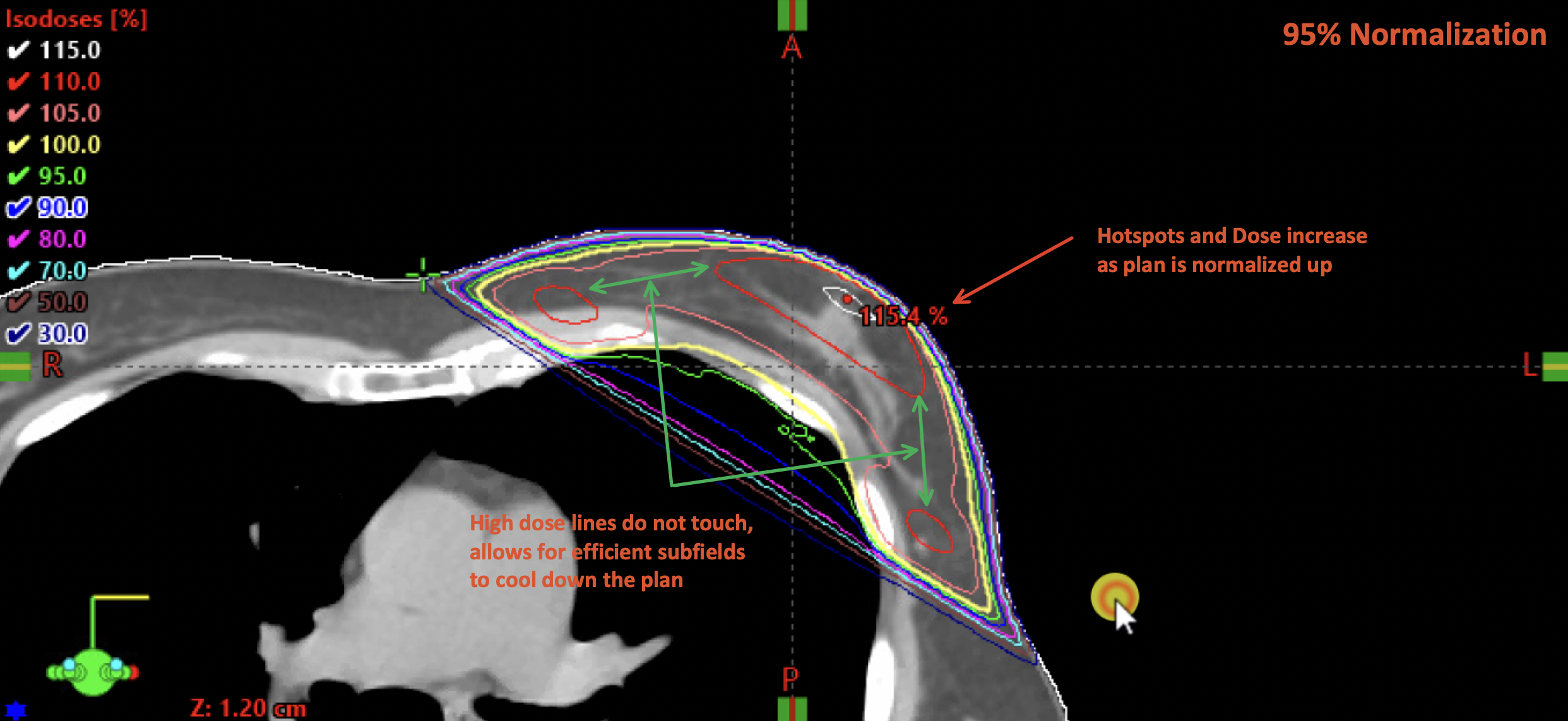
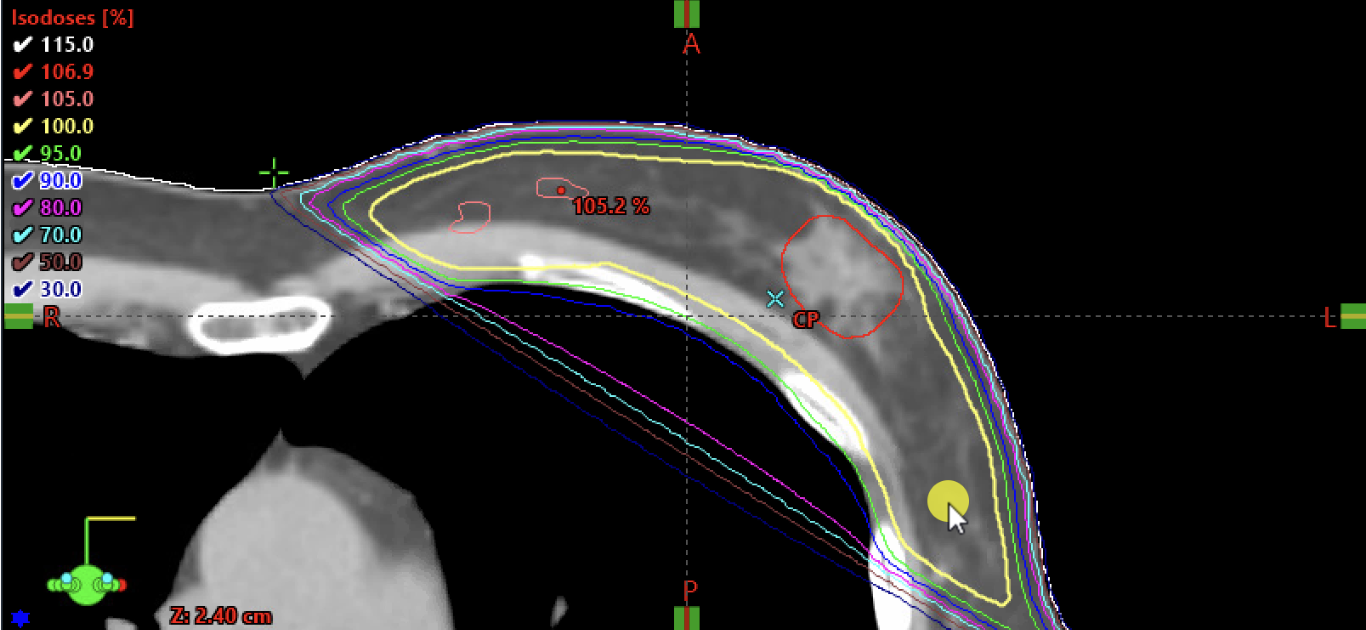
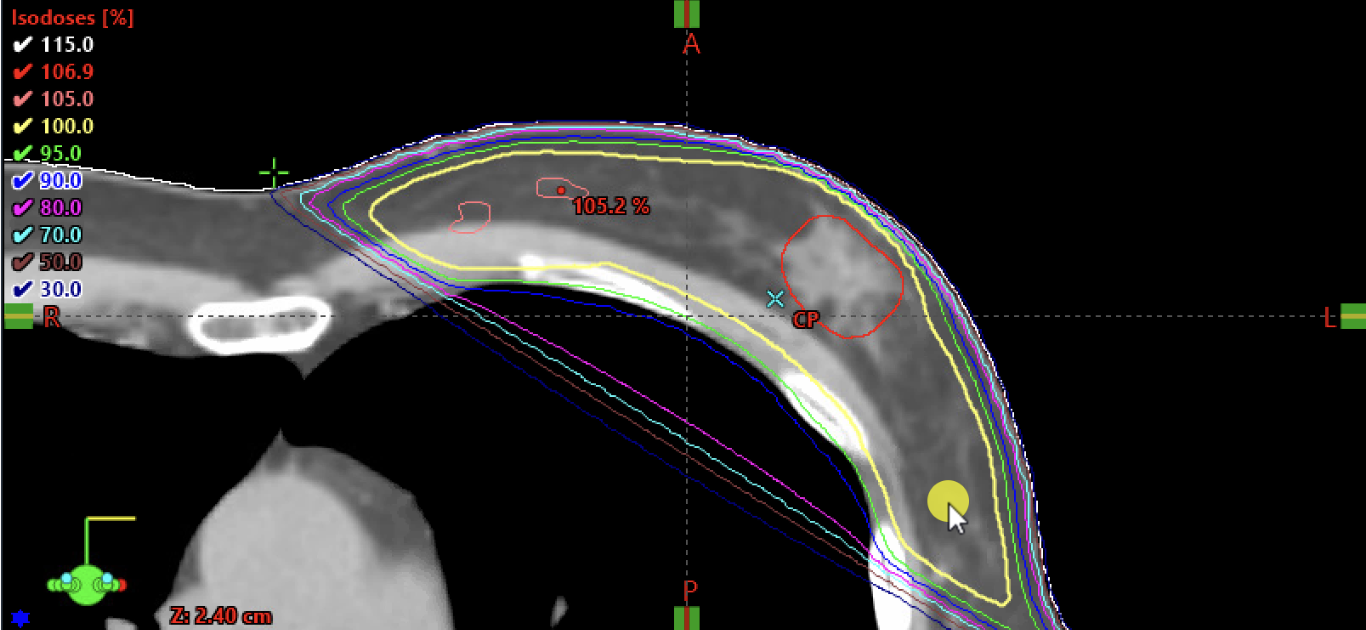
Plan normalization aims to optimize coverage so that the 95-100% isodose line closely conforms to the chest wall. Starting with an even distribution prior to normalization streamlines this process. Normalization scales the dose up or down to adequately cover the breast tissue.
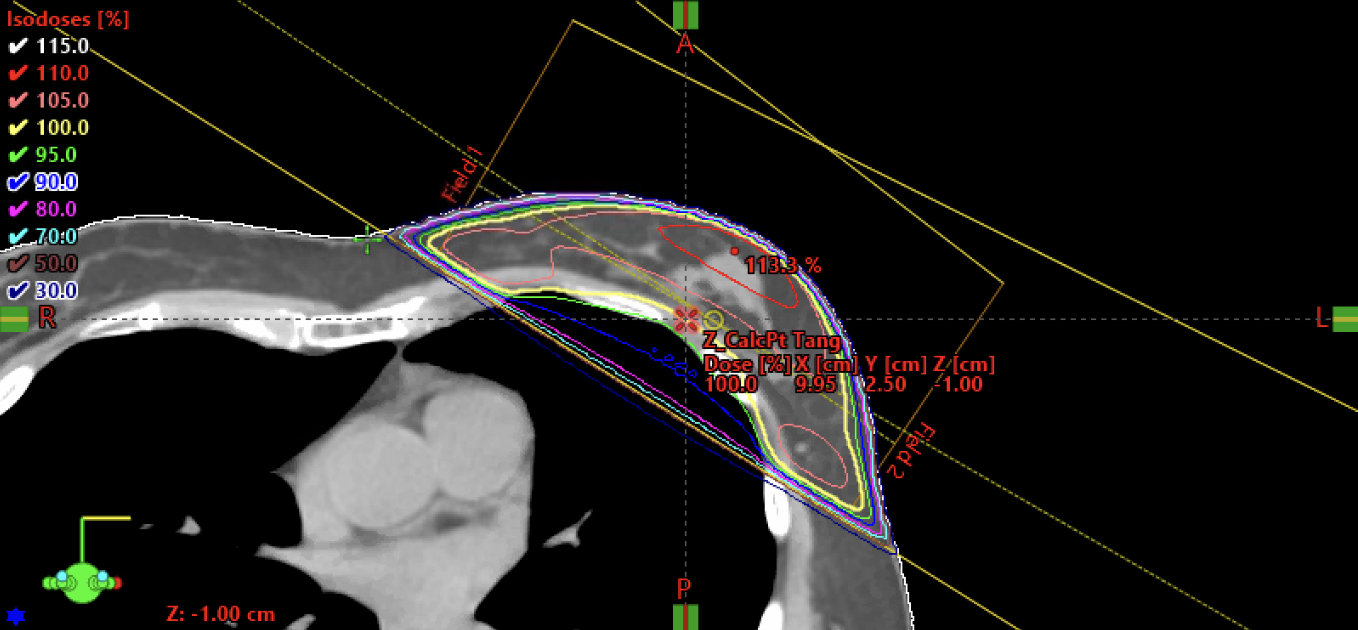
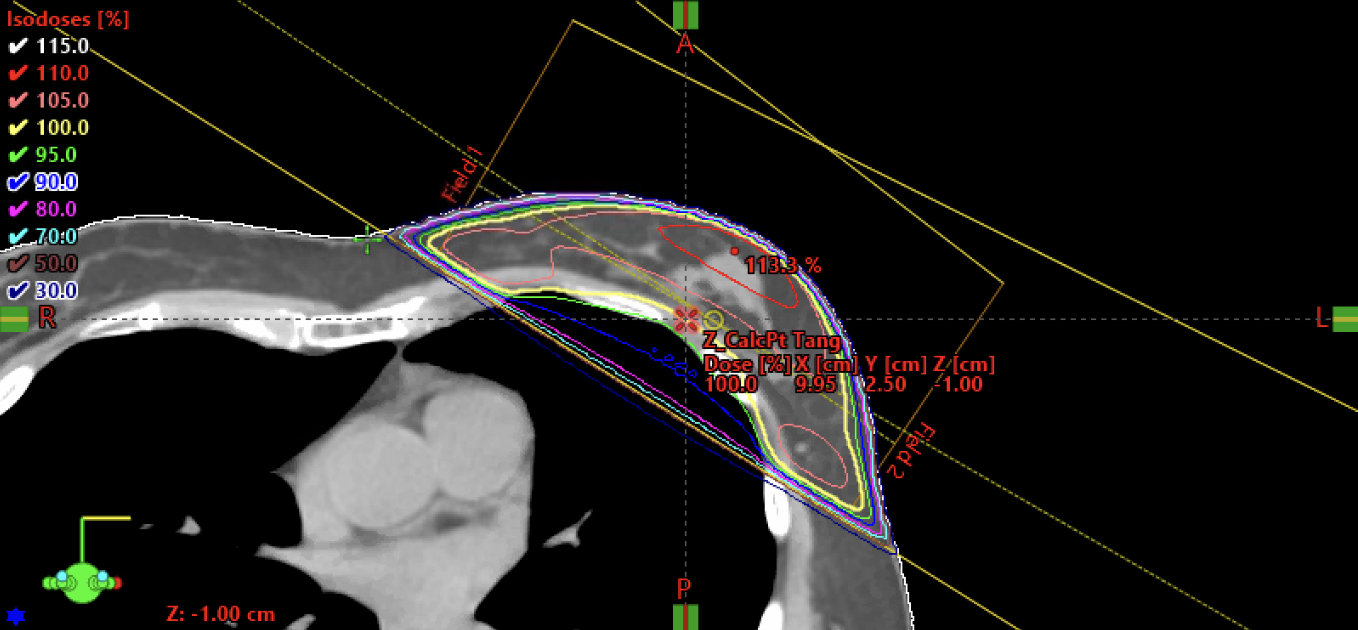
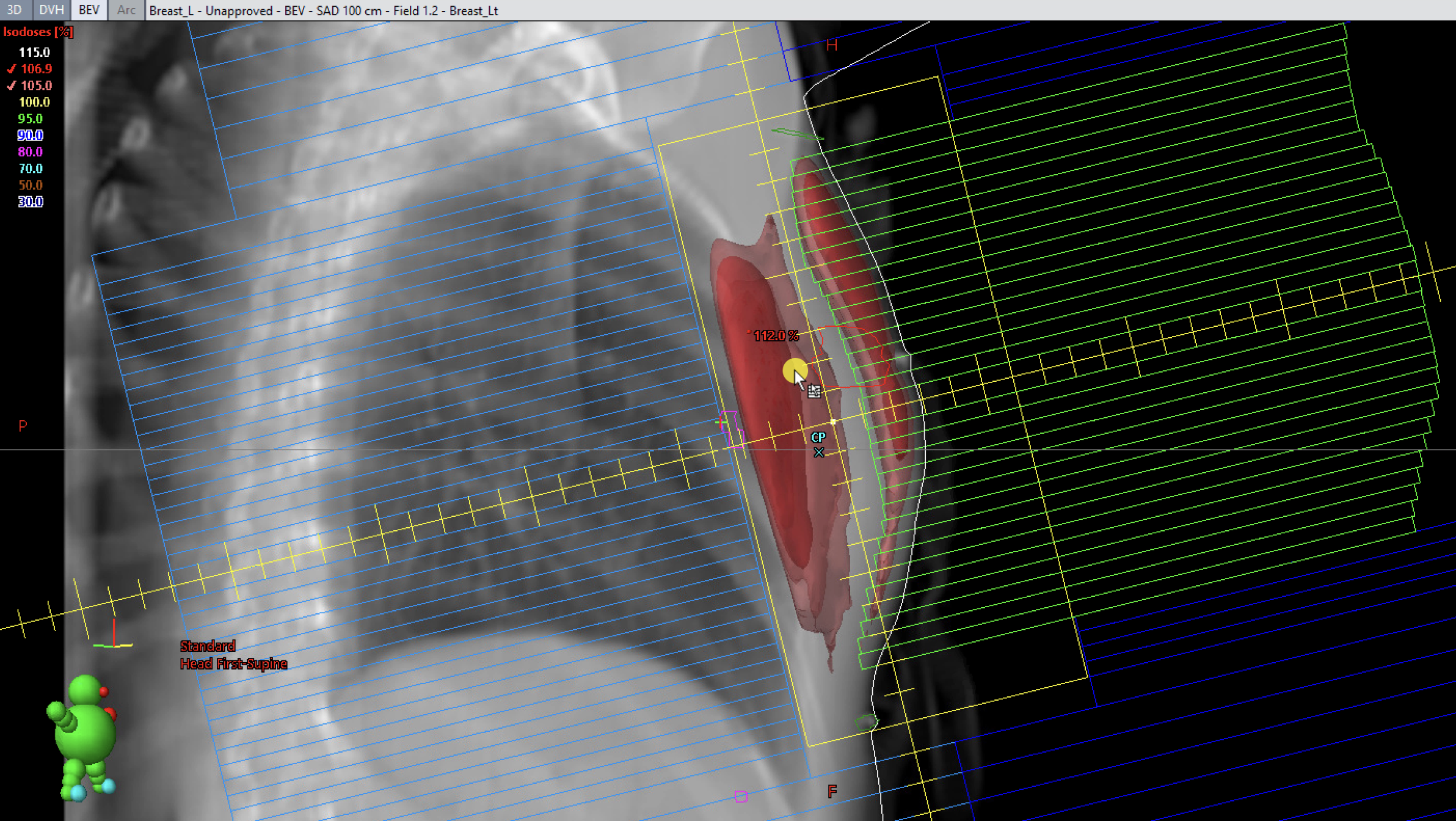
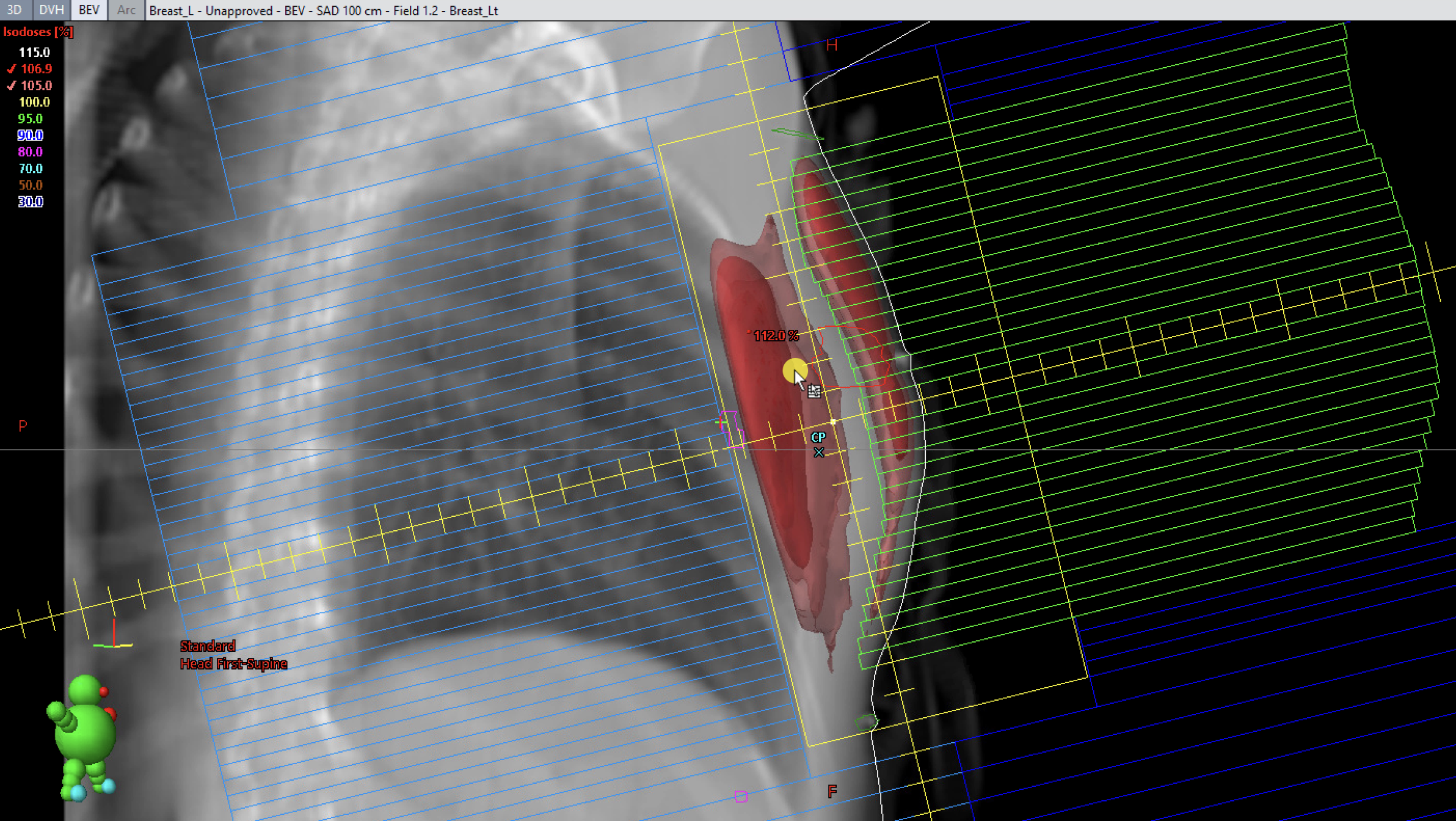
As the plan is normalized to improve coverage, monitor the maximum dose and the 110%-107% isodose lines in both axial views and the 3D Beam’s Eye View (BEV) isodose cloud (110% for standard fractionation and 107% for hypofractionation).
When examining the 3D dose cloud, ensure that the field is not entirely encompassed by the 110% (standard fractionation) or 107% (hypofractionation) isodose cloud, as shown below.
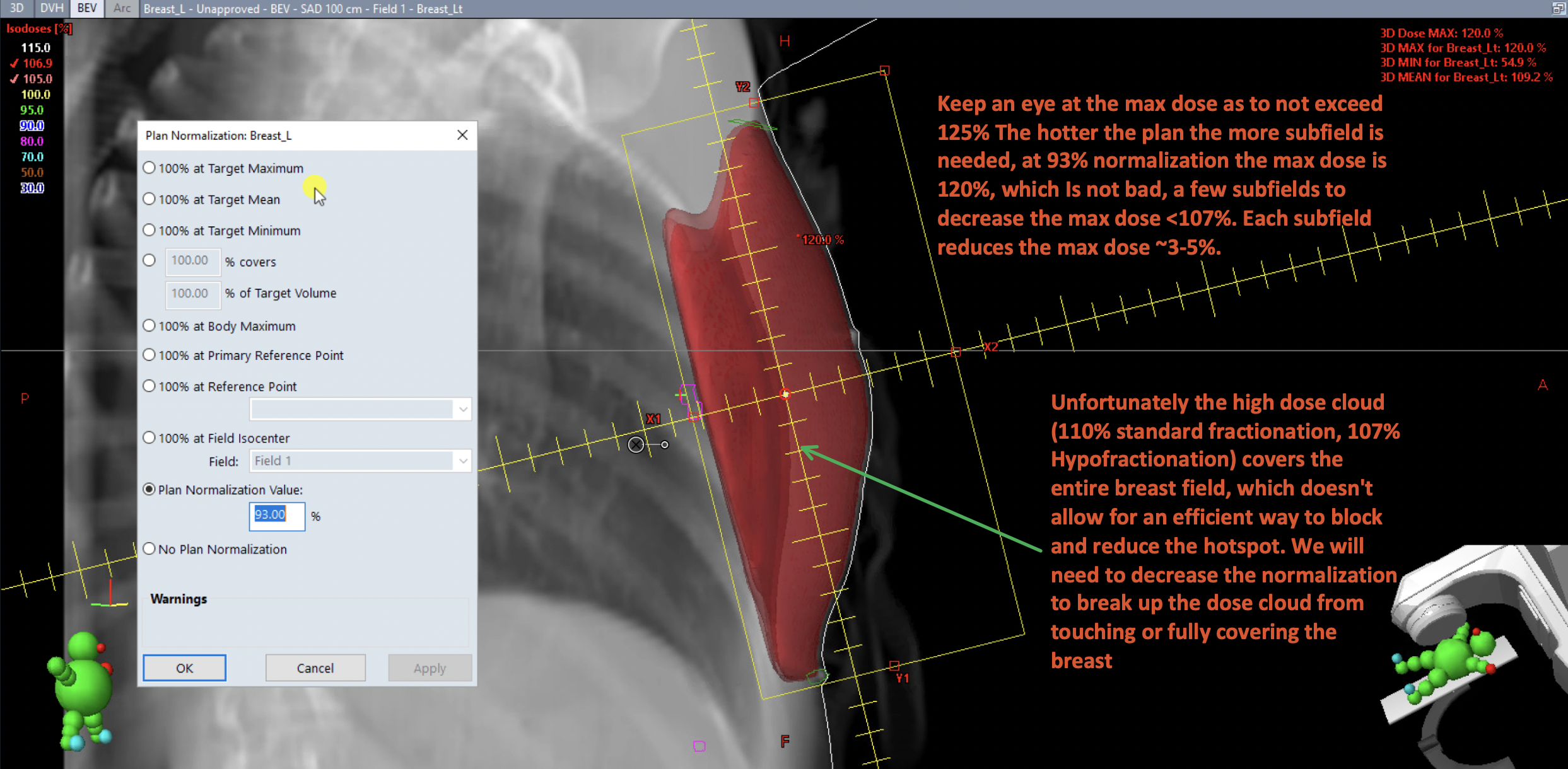
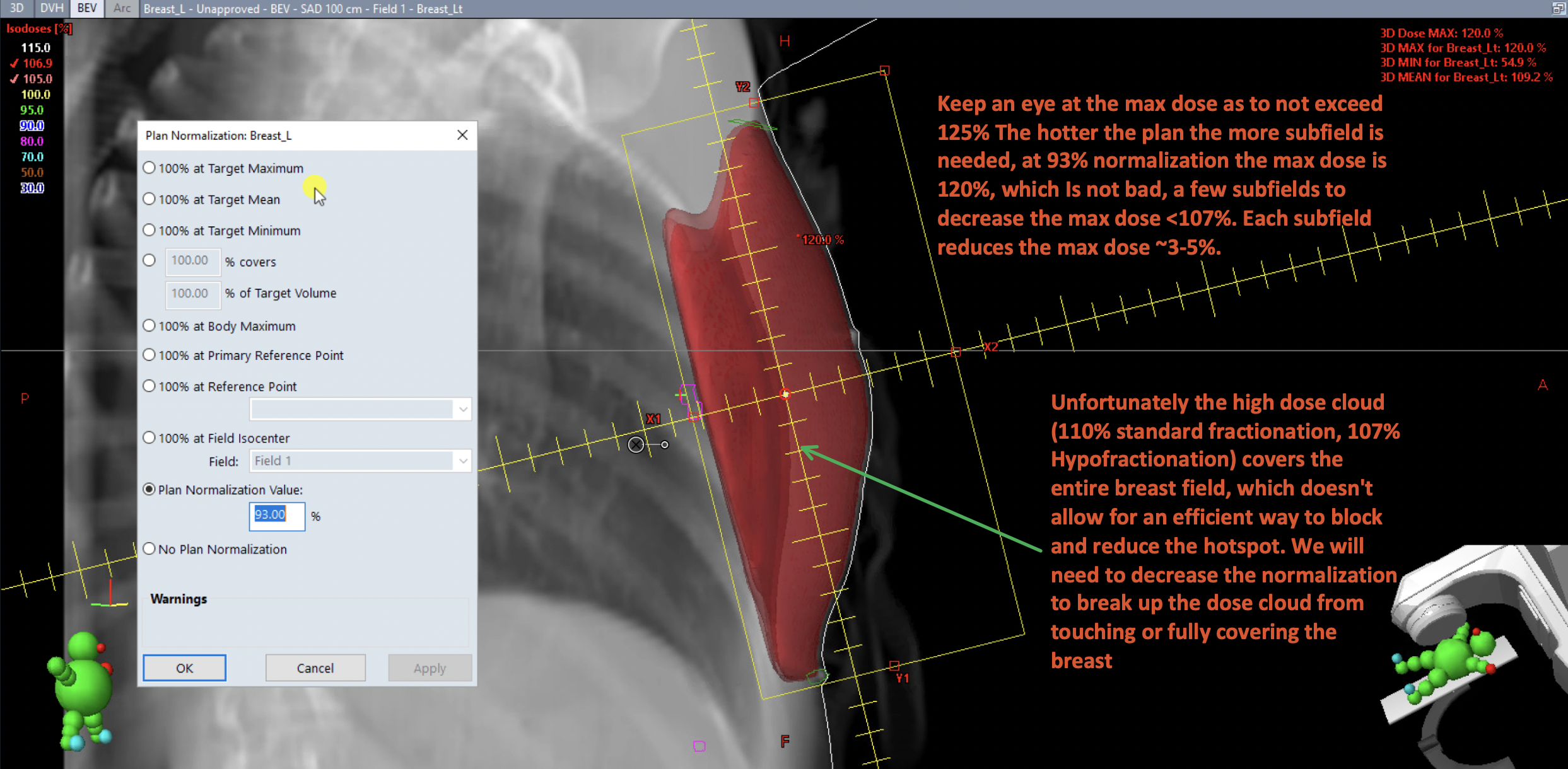
Monitor the maximum dose to ensure it does not exceed 125%. The higher the maximum dose, the more subfields are required. At 93% normalization, the maximum dose is 120%, which is acceptable; a few subfields can reduce it to below 107%. Each subfield typically lowers the maximum dose by approximately 3-5%.
If the high-dose cloud (110% for standard fractionation or 107% for hypofractionation) fully covers the breast field, it becomes challenging to efficiently block and reduce hotspots.
To address this, reduce the normalization to prevent the dose cloud from fully covering or touching the breast tissue.
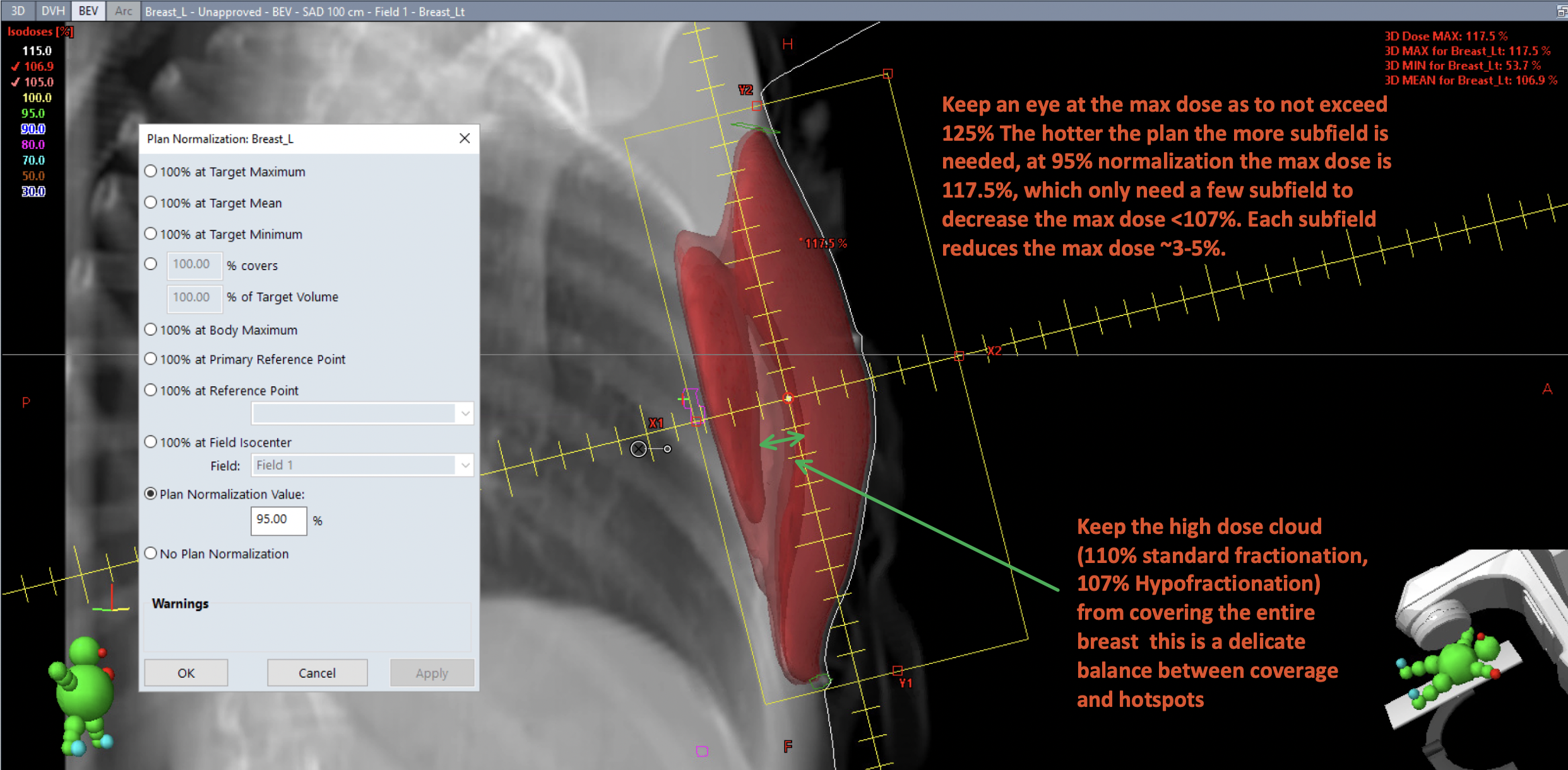
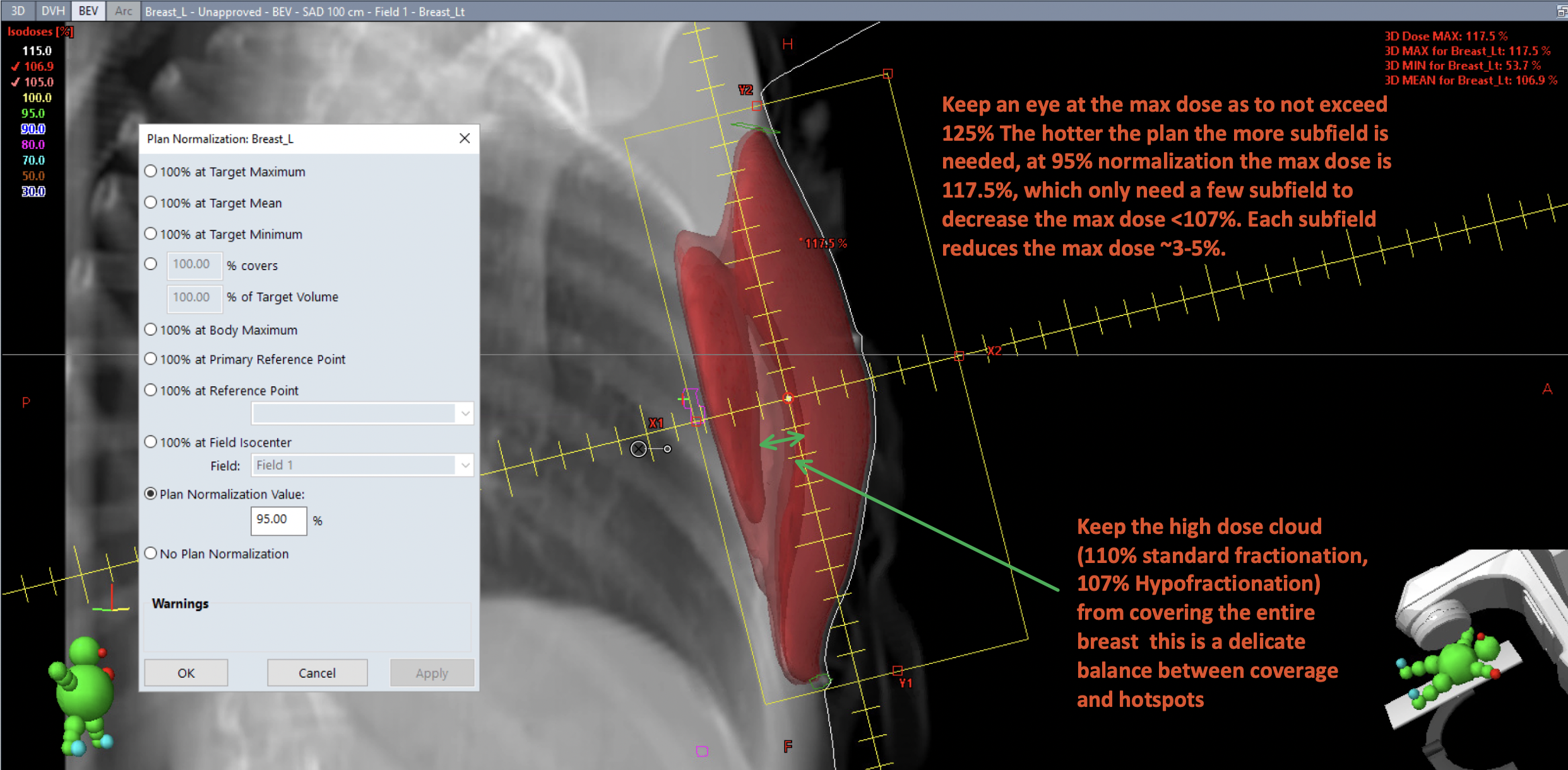
At 95% normalization, the maximum dose is 117.5%, and the 107% hotspots begin to separate slightly. This reflects a delicate balance between coverage and hotspot management. Maintaining gaps between the 107% isodose lines (for hypofractionation) or 110% isodose lines (for standard fractionation) enables multileaf collimators (MLCs) to block hotspots and reduce the plan’s overall heat.
Field Energy
To cover deeper targets, higher energy or mixed energies may be necessary. Typically, planning begins with 6 MV (6X) energy to preserve surface dose. For chest separations exceeding 22 cm, mixed energies may be introduced. Beyond 28 cm separation, achieving adequate coverage becomes challenging, even with higher energies such as 15 MV or 18 MV.
Planning involves a trade-off between coverage and hotspots/maximum dose. The goal is to keep the maximum dose below 110-108% for standard fractionation and below 107% for hypofractionation. Measuring chest separation during field setup aids in selecting the appropriate energy.
Field-in-Field Technique
When field weighting alone cannot eliminate hotspots, the field-in-field (FinF) technique—using subfields or control points—can reduce hotspots by selectively blocking parts of the field delivery. Below is an example of this approach.
Field-in-Field Process for Achieving Even Coverage and Reducing Hotspots
As subfields are added to mitigate hotspots, focus on blocking the high-dose regions (110% for standard fractionation or 107% for hypofractionation). Additionally, minimize the lower-dose hotspots (e.g., 105% isodose cloud in pink) at the apex as much as possible. Some 105% hotspots on the medial or lateral edges are generally acceptable. This process balances hotspot reduction with maintaining adequate coverage, prioritizing coverage unless otherwise directed by the physician.
Summary
Next, evaluate the plan to determine if it achieves the desired dose distribution and verify the maximum dose.
Next: Plan Evaluation

