Chapter 1 of 6
Simulation is a process that allows radiation treatment to be delivered in a reproducible manner. The simulator is a computed tomography (CT) scanner. The CT images are used to delineate targets as well as organs at risk, which allows the dosimetrist or physician to arrange the radiation beams and create a customized plan. Special care is taken to make the patient as comfortable as possible to ensure treatment can be delivered in the same position each day. Some considerations include:
Immobilization


Position: Supine
- Imaging: CT scan, typically ≤ 3 mm slice thickness
- Patients are positioned with both arms above the head.
- The patient’s chin should be raised and turned away from the treatment side.


- The patient should be inclined so that the sternal angle is as close to zero as possible to limit clearance issues.
- The physician places radio-opaque wires to delineate the superior, inferior, medial, and lateral field borders after the patient is properly positioned. The physician may also opt to place wires on incision sites.




Position: Prone
- The prone technique should be considered when treating a patient with pendulous breasts who does not require comprehensive nodal irradiation and whose tumor cavity is away from the chest wall. The purpose of this position is to reduce skin folds and to move target tissue away from the chest wall.
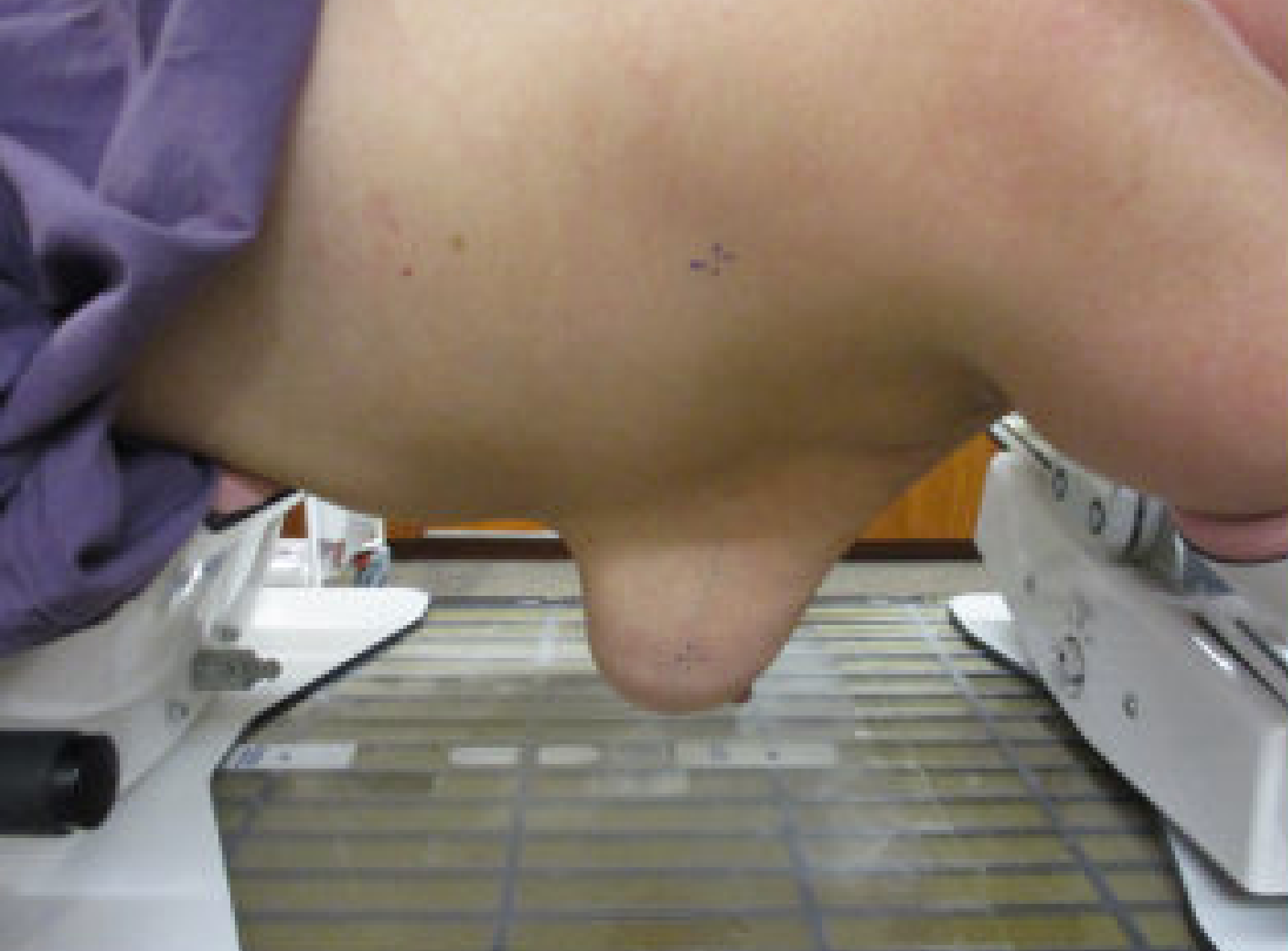
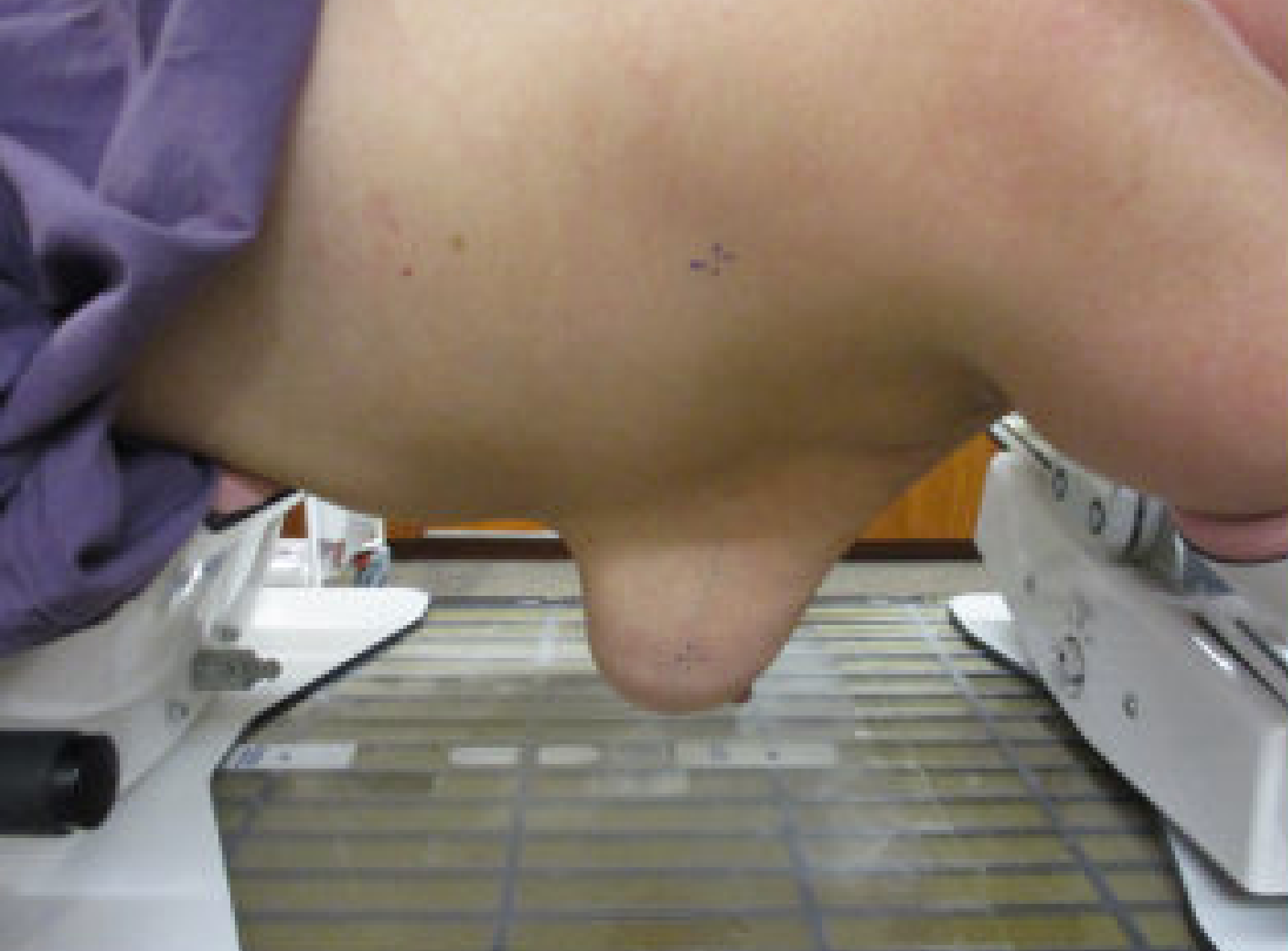
- The patient is set up prone on a specially designed immobilization device with both arms above the head, the ipsilateral breast falling anteriorly, and the contralateral breast displaced posteriorly away from the treatment fields.


- Patients treated in the prone position are usually treated with the opposed tangent technique. The treatment planning principles are the same as those used in the supine position, which will be discussed in a separate lesson module.
Motion Management
- For left-sided breast cancers, consider using the moderately deep inspiration breath hold (DIBH) treatment to reduce the dose to the heart.
- Moderately deep inspiration breath hold can be achieved using breathing control devices (e.g., ABC, RTP, lasers, VisionRT).
- Depending on patient-specific anatomy, not all patients undergoing DIBH will experience an increase in distance from the heart to the chest wall, and therefore a reduction in heart dose.
- Simulate the patient with and without breath hold and measure the distance from the edge of the heart to the chest wall.
Next: Import and Contouring

